What is Phantom Limb Pain?
Phantom Limb Pain (PLP) refers to painful sensations felt in a limb that has been amputated. It is a common and debilitating condition after limb amputation. PLP is as real as any other form of pain, even though the limb is no longer physically present. In fact, phantom pain can occur in other parts of the body that have been amputated, not only limbs. PLP can become chronic and more difficult to manage if left untreated. Fortunately, PLP can be treated and prevented in many cases!
Formal definition
Post-amputation pain encompasses Residual Limb Pain (RLP) and Phantom Limb Pain (PLP). The International Association for the Study of Pain (IASP) defines these pains based on their perceived location:
- Phantom limb pain is pain perceived in the missing limb.
- Residual limb pain is pain perceived in the residual limb.

For example, for a person with a below-elbow amputation, pain perceived in the phantom hand is categorized as PLP, and pain perceived in the forearm as RLP. A challenge when identifying PLP is that the position of the phantom limb is often different than expected. The phantom limb can be felt closer to the residual limb (known as "telescoping"). Sometimes, the phantom limb can be even felt within the residual limb itself, which can lead to misidentification. Special attention when describing post-amputation pain is recommended in such cases. Pain perceived in the phantom limb is PLP although the phantom limb is perceived within the residual limb. In the aforementioned example, pain in a phantom hand perceived within the residual forearm is considered as PLP. In the case in which there is no perception of the phantom limb, no post-amputation pain is considered PLP. It is important to distinguish between different types of post-amputation pain, as each may require a different treatment approach!
What is Neuroma Pain?
Another form of post-amputation pain is neuroma pain, which is pain caused by the stimulation of symptomatic neuromas. The endings of amputated nerves form neuromas when left untreated, and these neuromas can cause pain when disturbed. Keep in mind that not all neuromas cause pain (asymptomatic neuromas), and there can be several neuromas in the residual limb. Pain caused by neuromas can be perceived in the residual and/or phantom limb, and therefore contribute to either or both RLP and PLP, as per their definition.
Because PLP can be caused by different reasons, it is important that the ones present in a particular patient are identified and properly addressed for effective treatment. There are specific treatments for painful neuromas that do not necessarily alleviate PLP, and treatments for PLP that do not resolve neuroma pain.
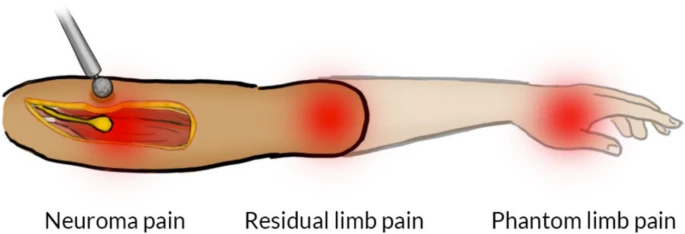
Image from Pettersen et al., Trials, 2023.
What counts as Pain?
Not all sensations in the phantom limb (or Phantom Limb Sensations - PLS) are painful, for example, the presence, position, and movement of the phantom limb are often described as non-painful. The IASP defines pain as:
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”
PLP are therefore sensations fulfilling the description of pain perceived in the missing limb. Because PLP is caused by an amputation, and therefore due to nerve damage, PLP is part of neuropathic pain defined as:
"Pain caused by a lesion or disease of the somatosensory nervous system"
PLP can also be described as neuropathic pain perceived in the missing limb. However, since all PLP is neuropathic pain, the "neuropathic" descriptor is often omitted.
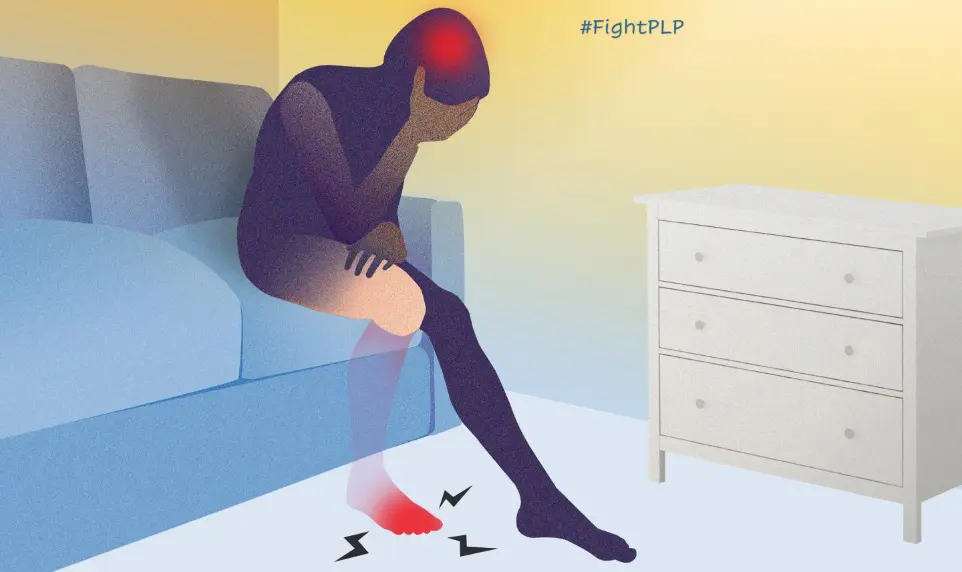
How does PLP feel?
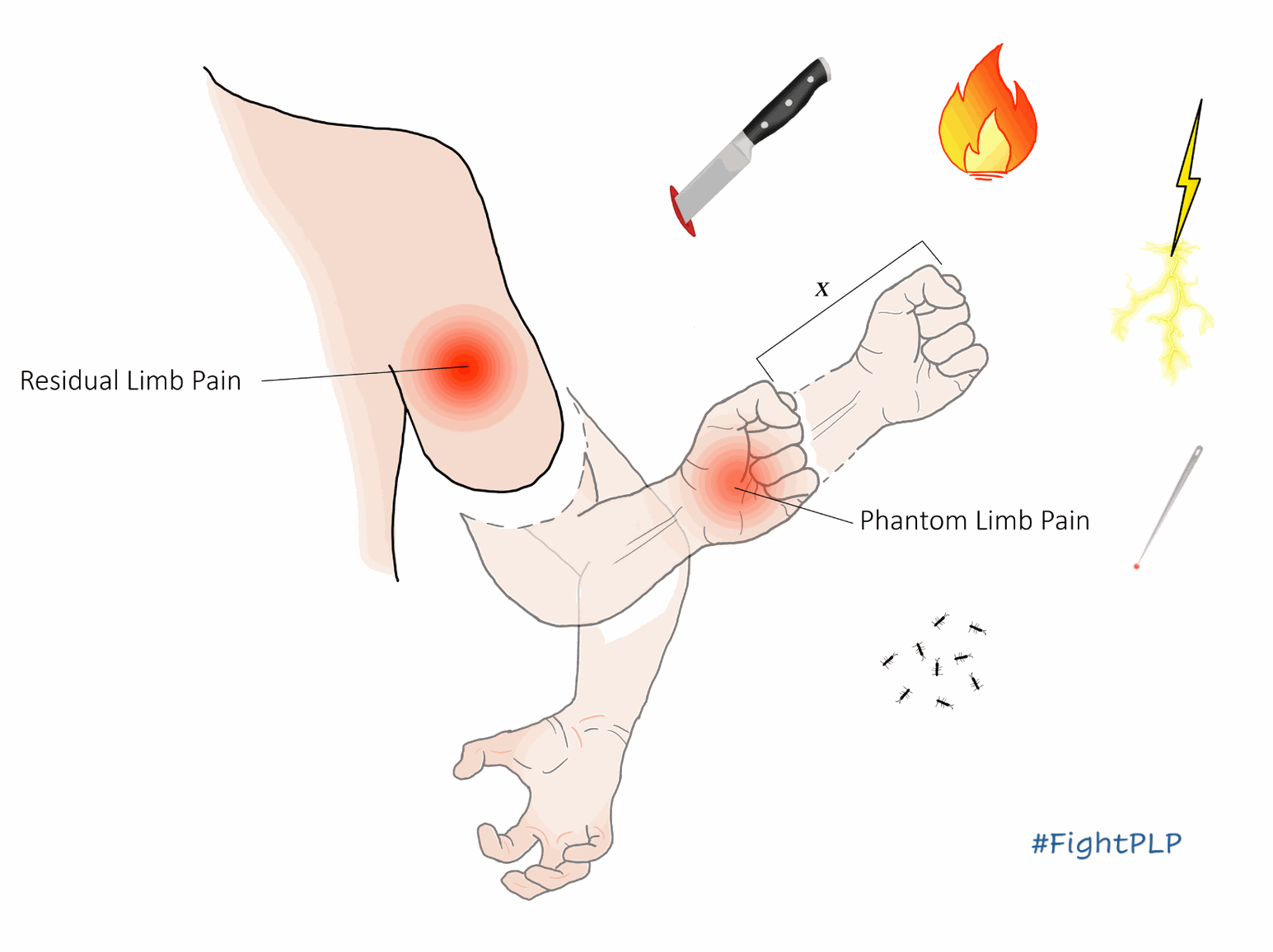
PLP is experienced as any other pain in in the body. Descriptions often used are burning, stabbing, shooting, cramping, etc. In addition, the position of the phantom limb can be perceived in anatomically painful posture, such as bent backwards. It is common for people to feel their phantom limb "locked" or "frozen" in place, which prevents them from moving it away from painful postures. Fortunately, there are treatments that can help returning mobility to the phantom limb.
Acute or Chronic PLP?
PLP can be felt momentarily (acute) or for long periods of time (chronic). The rule of thumb to consider pain as chronic is to experience it for over 3 months. The frequency of pain does not normally count for chronicity, for example, PLP that is felt all the time, or every other day for over 3 months, are both considered as chronic, regardless of how often it occurs.
What is the impact of PLP?
PLP can considerably affect the quality of life of the sufferer and it's known to have a negative impact in employment, social participation, and practically in all aspects of life. More information to come...
How common is PLP?
PLP is experienced by most people with amputations. More information to come...